Goldilocks: the Middle Way

Skip to Section:
Oncoplastic techniques to remove all redundant (excess) tissue and create a smooth contour go a long way to producing results patients can live with. But even with a dedicated and highly skilled oncoplastic surgeon, and/or plastic surgeon using traditional techniques, patients can be left with significant concavity (looking “scooped out”).
In a Goldilocks procedure, instead of removing the redundant tissue, the surgeon instead rearranges it over the mastectomy site to rebuild either a flat chest wall contour with minimal or no concavity or a small recognizable breast mound.
In the story of Goldilocks and the three bears, the first porridge she tries is too hot, the second too cold, and the third just right.
A Goldilocks mastectomy is the “middle ground” between traditional breast reconstruction that requires implants and/or autologous flaps and traditional non-reconstructive mastectomy. It’s “just right” for some patients!
Minimizing Concavity After Mastectomy or Explant
Many (not all) patients are unpleasantly surprised when they wake up from their mastectomy surgery without conventional reconstruction to find that their chest wall is actually concave, or “scooped out,” rather than smooth and flat. Concavity is mostly due to the patient’s anatomy, i.e., the rib cage and the overlying musculature, and can be more pronounced after explant.
Examples of Concavity



(and excess skin)



There is no way (short of medical imaging, which involves risk and expense and would not be covered by insurance) for the surgeon to anticipate the degree of concavity for a specific patient. To set expectations, many surgeons will mention that concavity is a possibility. But it can be hard for patients to visualize what this means for their own bodies, and waking up concave can be jarring.
There are two ways to surgically address concavity for a patient who does not want to reconstruct breast mounds. Local tissue rearrangement is done at the time of the initial surgery, and fat grafting is done later. Since most patients going flat want to be done in one surgery, it is usually preferable to use local tissue arrangement. There are many types of relatively simple tissue rearrangement techniques.
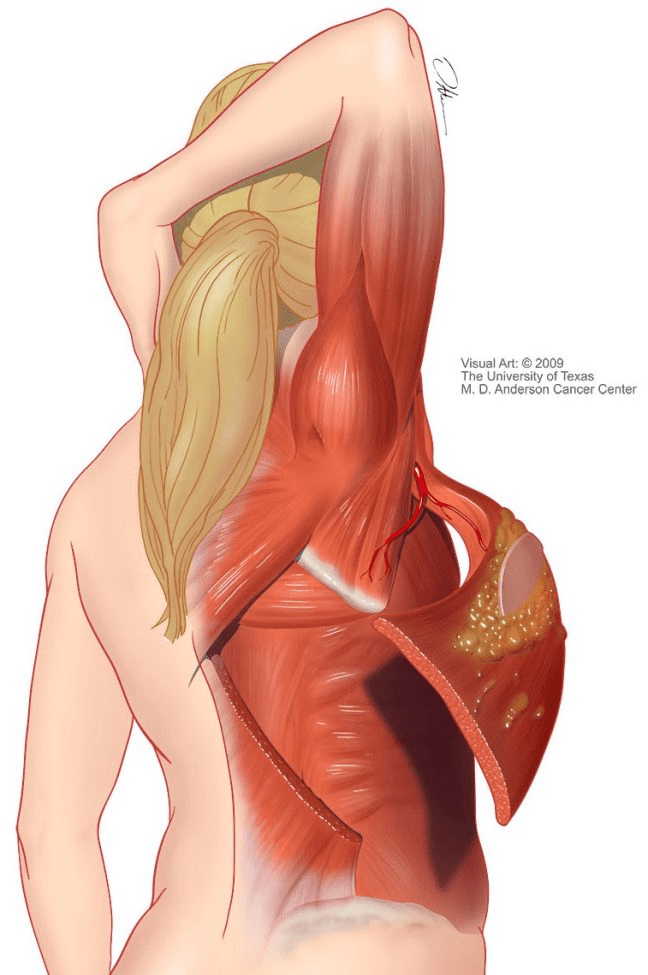
Goldilocks takes local tissue rearrangement one step further. With this technique, the breast tissue is removed carefully to preserve blood flow to the maximum amount of surrounding, healthy excess fat and skin. The healthy tissues are then rearranged over the mastectomy site. When only a small amount of tissue is available, the result may be simply a flat chest with minimal or no concavity (below, right). With a large amount of tissue, the surgeon may be able to create a small breast mound – if the patient so desires (below, left).

Patients with large, pendulous breasts

Patients with smaller breasts
Goldilocks Photos



















Why Choose Goldilocks?
All reconstruction options are equally valid choices. This section explains why some women may choose to go flat or have Goldilocks instead of conventional breast reconstruction or conventional “non-reconstructive” mastectomy. Choice is a beautiful thing!

SOURCE: M.D. Anderson
SOURCE: M.D. Anderson

SOURCE: Parker Center for Plastic Surgery
But patients who reject conventional breast reconstruction still care about how they look, and a smooth flat contour is both more aesthetically pleasing AND more comfortable than a concave or discontinuous/”lumpy” contour. Goldilocks can be an excellent option to maximize cosmesis for those patients who prioritize cosmesis and find a somewhat longer anesthesia burden to be acceptable.
Who is a Candidate for Goldilocks?
Any patient who is a candidate for a skin-sparing mastectomy from an oncologic perspective is technically a candidate for Goldilocks, whether they are interested in producing a recognizable breast mound or just having a smooth chest wall contour. Patients who are explanting their implant reconstruction may be candidates for similar tissue rearrangement to counteract potential concavity.
Patients with very large or pendulous breasts have significant redundant fatty tissue and skin for the surgeon to work with are more likely to be able to achieve a recognizable breast mound.
Risks & Benefits
Risks. While there is no long-term data on the oncologic safety of Goldilocks, surgeons offering this procedure say that the oncologic and surgical risks are similar to that of a skin-sparing mastectomy. The reason is that Goldilocks is a skin-sparing mastectomy performed in such a manner that the remaining redundant tissues can be rearranged in order to produce either a recognizable breast mound or a smooth chest wall contour to minimize concavity caused by the removal of the glandular tissue. Preserving the tissues and doing so in a way that preserves the blood supply, as well as rearranging the tissues, all take extra time in the operating room. Extra time under anesthesia carries with it proportional increased risk.
Benefits. Goldilocks typically results in improved chest wall aesthetics (minimal or no concavity) and avoids implants and distant donor sites.
We do not have data on patient-reported outcomes or quality of life after Goldilocks mastectomy versus other types of breast or chest wall reconstruction. However, Goldilocks does typically improve concavity, which is one of the main cosmesis complaints that patients going flat have – particularly when they were not anticipating seeing a concave contour.
Anecdotally, most of the patients in the flat community online report that they are very happy with their choice to have a Goldilocks procedure. There’s a relatively new Facebook group for Goldilocks information sharing and support here.
Who Performs Goldilocks Surgery?
A Goldilocks mastectomy is an oncologic surgery, and the surgeon performing your mastectomy must be a cancer surgeon – that is, a surgical oncologist, general surgeon, or breast surgeon. The cancer surgeon may also do the tissue arrangement themselves, or they may enlist the services of a plastic surgeon. Sometimes the plastic surgeon helps plan the incisions, and then the cancer surgeon performs all the surgery themselves.

You can search for a surgeon who offers Goldilocks on our Flat Friendly Surgeons Directory by checking the checkbox marked “Goldilocks.”
Note: most surgeons do not offer this procedure. It can be technically complex and requires specific training as well as additional operating room time. However, it’s important to note that many surgeons, particularly breast specialists and those with oncoplastic training, may offer similar or related procedures (see next section).
Related Procedures
V-Y Plasty & De-Epithelialization
There are many variations on local tissue rearrangement that can be used to produce an aesthetic flat closure. In addition to Goldilocks, the popular v-y plasty is used to minimize dog ears under the arms and results in a y-shaped incision. To address concavity for patients who have minimal redundant fatty tissue, a procedure called de-epithelialization can be performed on the excess skin and it can then be folded under to create padding before closing the primary mastectomy flap. This is often done after explant, because the mastectomy flap is typically quite thin and was spared during the initial mastectomy, so it’s available to be used for rearrangement.
Fat Grafting
Autologous fat grafting is a procedure where subcutaneous fat is liposuctioned from a donor site on your body, treated, and then injected under your skin in an area the surgeon wants to “bulk up.” Radiation fibrosis adhered to the chest wall, divots, and areas of concavity are some examples where fat grafting may be used to optimize the cosmesis of a flat closure. Fat grafting is not performed at the initial mastectomy, but at a later date, and sometimes can require multiple procedures. If you decide to pursue fat grafting, it’s critical to choose a surgeon who has a lot of experience with the procedure in order to maximize your chances of success. (Read More)
Questions to Ask Your Surgeon
Since the end result of a Goldilocks procedure is largely dependent on the amount and quality of tissue the surgeon has to work with, your surgeon may not be able to tell you in advance exactly what your result will look like. The exact location and integrity of the blood supply, the presence of additional disease, and other factors can affect your ultimate aesthetic outcome. Be clear with your surgeon about your goals:
- Contour Preference. Do you want a flat chest, or do you want a breast mound? This is an important conversation to have because if you prefer to have a flat chest, it must be clear that that is your goal in the event that additional tissue is available to produce a breast mound. Ask your surgeon to explain to you what you should expect in terms of your final contour.
- Nipples. Are you interested in preserving any part of the nipple area or complex? Depending on your medical situation, you may be eligible for a nipple-sparing procedure or an areola sparing procedure.
- Are you interested in surgical nipple reconstruction? If so, will the surgeon perform that reconstruction at the time of the mastectomy or will you need a separate surgery? What about restorative tattooing?
- Incision Pattern. Will they be using a wise pattern incision (resulting in an anchor pattern scar, with or without nipple grafts)? If not, why not? Do you have a preference for your scar pattern?

Read More: Preparing for Your Surgery
Read More: Going Flat After Mastectomy
Read More: Going Flat at Explant
Frequently Asked Questions (FAQ)
The few online resources that showcase Goldilocks frame it exclusively as a type of breast mound reconstruction. You won’t find many (if any) pictures of Goldilocks resulting in aesthetic flat closure at present. That’s because until very recently, very little attention was paid to the aesthetics of patients going flat. But that’s changing now, and we hope to see surgeons showcasing their own flat closure pictures soon!
Any patient who is a candidate for a skin-sparing mastectomy from an oncologic perspective is technically a candidate for Goldilocks. Ask your surgeon about your specific medical situation.
Because it is in between traditional breast reconstruction and going flat. In the story of Goldilocks and the three bears, the first porridge she tries is too hot, the second too cold, and the third just right. In planetary science, a Goldilocks planet is just the right distance from the star (sun) it orbits to allow for life to evolve – not too close, not too far. A Goldilocks mastectomy is the “middle ground” between traditional breast reconstruction that requires implants and/or autologous flaps and traditional “non-reconstructive” mastectomy. It’s “just right” for some patients!
It can be, but it doesn’t have to be. The Goldilocks procedure can be used to produce a recognizable breast mound, but it can be also used to produce an aesthetic flat closure. The outcome depends on the patient’s goals, and on how much extra tissue is available for the surgeon to work with. With very little tissue, the result may be less or even no concavity. With a lot of tissue, the result may be a recognizable breast mound.
Note: Goldilocks is currently advertised exclusively as a type of breast reconstruction because it was first performed on patients with very large and pendulous breasts with the goal of producing a recognizable breast mound. Historically, the idea of employing plastic surgery techniques for a patient going flat was not widely considered or accepted. Thankfully, that is changing now.
The surgeons who offer this procedure typically say that the risks are similar to skin or nipple-sparing mastectomy. But there’s no long-term data on the oncologic safety of Goldilocks specifically.
It can be, if the patient is otherwise a candidate for nipple-sparing – but it doesn’t have to be. The procedure can be performed with or without saving the nipple and/or areola. Note: Most patients who are not candidates for nipple-sparing, are eligible for nipple reconstruction. That can involve surgical reconstruction of the nipple and/or restorative tattooing and is typically covered by insurance.
It varies, but it’s on the order of 1-3 hours. Compare that with an autologous flap reconstruction which can take six hours or more.
Both procedures are types of local tissue rearrangement, but they serve different functions and result in different scar patterns. A v-y plasty is done to minimize “dog ears” under the arms but does not necessarily address concavity where the breast tissue was removed and results in a y-shaped scar with the fork under the arm(s). In a Goldilocks procedure, tissue is rearranged over the mastectomy site in order to bulk it up (to minimize concavity, or to produce a breast mound). Goldilocks typically uses a “wise pattern” incision which results in an anchor-shaped scar with or without a repositioned nipple/areola.
Lumpectomy preserves breast tissue, Goldilocks mastectomy does not. In a lumpectomy, the disease (tumor) is removed but the rest of the breast glandular tissue is preserved. In an oncoplastic lumpectomy, this excision is done in such a way to reshape the breast contour and optimize cosmesis, and is often combined with a contralateral breast reduction to achieve symmetry. In a Goldilocks mastectomy, similar tissue arrangement techniques are used, but all of the breast glandular tissue is removed to the greatest extent possible.
In local tissue arrangement, the blood vessels supplying the tissue being moved are largely preserved during the surgery. This requires that the surgeon take meticulous care planning the excision and handling the tissues and is one reason the procedure takes longer than a “non-reconstructive” mastectomy without tissue rearrangement.
You can visit the Photos section on this page.
You can search our Flat Friendly Surgeon’s Directory and check the “Goldilocks” checkbox to filter for those surgeons offering the procedure. We currently have only a handful of such surgeons on our Directory, and we are hoping that grows over time.
A Goldilocks mastectomy is an oncologic surgery, and the surgeon performing your mastectomy must be a cancer surgeon – that is a surgical oncologist, general surgeon, or breast surgeon. The cancer surgeon may also do the tissue arrangement themselves, or they may enlist the services of a plastic surgeon. Sometimes the plastic surgeon helps plan the incisions, and then the cancer surgeon performs all the surgery themselves. Other times the plastic surgeon may be present in the operating room to perform the closure (this is a “co-surgery”).
Absolutely! You can apply to be listed on the Directory by filling out the short form here. You can find more resources on aesthetic flat closure here.
SWIM is an acronym for Skin-sparing Wise-pattern Inframammary Perforator, which is a synonym for Goldilocks used by some surgeons and describes the main blood vessel preserved in a Goldilocks mastectomy.
Further Reading
Meet The Brains Behind The Goldilocks Mastectomy and SWIM Breast Reconstruction
SWIM Flap Breast Reconstruction – Cassileth Plastic Surgery
Goldilocks Mastectomy – The Bedford Breast Center
The Goldilocks Mastectomy, Richardson, H., 2012
Quick Links
| Apply to be Listed Directory | Recommend Your Surgeon | Going Flat: Guide | Find a Surgeon |
| Order Brochures | FAQ (Patients) | FAQ (Providers) | Explanting |
| Photo Gallery | Donate | Blog | Contact Us |
Find out more!

REGISTERED CHARITY ID# 84-3021062
FAIR USE STATEMENT
This site contains copyrighted material. Not Putting on a Shirt’s educational materials and resources on this site are freely available for “fair use” (Title 17 U.S.C. Section 107) in accordance with our mission to advocate for optimal outcomes for those who choose to go flat after mastectomy. The copyrighted material on this site is distributed for educational purposes without profit – all donations to Not Putting on a Shirt directly fund our advocacy work. If you wish to use copyrighted material from this site for purposes that go beyond “fair use”, you must first obtain explicit permission from the copyright owner. Please direct requests or questions to info@notputtingonashirt.org.
